Relationship Between Depression and Blood Pressure and Pulse Rate in an Adolescent Clinic
AUTHORS:
Esraa M. Eloseily MD1,2; James J. Burns MD MPH1; Raid Amin PhD3; John Bruyere MD1; Steffi Khurana MD1; Ali Kurady MD1
1Department of Pediatrics, University of Florida, Pensacola, FL
2Department of Pediatrics, Assiut University, Assiut, Egypt
3Department of the Mathematics and Statistics, University of West Florida, Pensacola, FL
resident article | PUBLISHED SUMMER 2022 | Volume 42, Issue 3
DOWNLOAD PDF
Abstract
Background
Depression is a risk factor for adult cardiovascular mortality with unclear pathophysiology. The literature on physiologic parameters related to depression is inconsistent and scant in adolescent patients.
Aim of the study
The purpose of this study is to determine if there is a relationship between depression and physiologic parameters including blood pressure (BP) and pulse rate (PR) in adolescents.
Methods
Adolescents with and without depression were compared to controls without depression for systolic BP, diastolic and PR using a two-way type III ANOVA.
Results
In depressed patients, there was significantly higher systolic BP percentiles (57.4 depressed versus 47.8 non-depressed; F (DF 1) = 4.48, p = 0.036), no difference in diastolic BP, and significantly higher PR in depressed males but not females (males depressed 86.7 vs. 72.1; F (DF 1) = 8.61, p =0.003).
Conclusion
Significantly higher systolic blood pressure percentiles in depressed patients vs. non-depressed patients and significantly higher pulse rates in depressed males but not females were found. These findings may lead to a greater understanding of the physiologic correlates of depressive psychopathology that have implications for subsequent development of cardiovascular disease.
Keywords: Hypertension, Heart rate, Adolescents, Depression
Introduction
Psychiatric disorders are associated with pathological, physiologic, or subclinical evidence of accelerated atherosclerosis.1,2,3 Anxiety and depression, has been associated with an increased risk of cardiovascular disease.2,4-8 Evidence suggests that the risk of mortality is increased in patients with coronary artery disease who have comorbid depression.9,10
Major Depressive Disorder and Bipolar Disorder have been categorized as tier II (moderate) cardiovascular disease risk factors by the American Heart Association.11 Further study of the relationship between psychiatric diseases and cardiovascular disease (CVD) risk factors in children and adolescents is needed.
Mental health problems affect pathophysiological pathways with increased oxidative stress, inflammation, and autonomic dysfunction.12 Oxidative stress is related to the progression of CVD and, is also frequently increased in patients with psychopathology.11 Inflammation, an established known factor in the pathogenesis of CVD, was also found to have a bidirectional relationship with depression and childhood adversity.11,13 Also, depressed patients were found to have worse autonomic function compared to those without depression, and it is thought that dysfunction may result in many long-term complications, such as hypertension in young individuals.14 Therefore, the combined long-term effect of these different pathophysiological changes is hypothesized to enhance the progression of CVD in patients with psychopathology.11
Hypertension is a significant risk factor for CVD,15 and evidence suggests that it could be more common among patients with psychopathology.16 Therefore, hypertension could explain part of the long-known association between psychopathology and CVD.17 Studies investigating the association between BP and anxiety and depression have had inconsistent results ranging from a positive association,18 a negative association,19 or even a nonexistent association.20 The same level of controversy with even more scarce studies is found in the adolescent population.21
Looking at sex differences, most of the studies showed that the blood pressure had no significant sex differences in association with depression, despite higher scores of depression in women and higher blood pressure in men.19 One study showed that the relation between blood pressure and depression was only in boys.22 Additionally, the Baltimore Longitudinal Study of Ageing showed lower blood pressure in men with depression, but the inverse relationship in younger women.23
The purpose of this study is to further analyze the relationship between depression and BP or P in adolescents. The hypothesis is depression will be related to higher BP and PR.
Methods
Prior to data collection, approval was obtained from the Sacred Heart Hospital Institutional Review Board (IRB).
Inclusion criteria: This case-control study included patients over age of 13 years, who attended an Adolescent Medicine outpatient residency teaching clinic. Patients who were diagnosed with a depressive disorder were compared to a control group without a depressive diagnosis for systolic and diastolic BP percentiles (derived from CDC age and sex data) and pulse rates. The patients attended the clinic for various reasons including well child visits, sports physical exam, visits for acute medical or mental health problems. Patients from both groups were randomly selected from a three-year period 12/2015 to 12/2018. Diagnosis of depression was made by the same board-certified Adolescent Medicine subspecialist using the Diagnostic and Statistics Manual of Mental Disorder (DSM-V) criteria based on direct interview and assessment of function and distress with information provided by the Patient Health Questionnaire-9 (PHQ-9) score. Since this was a retrospective chart review, ID-10 diagnostic codes F32.0-F32.9, F33.0-F33.9 were used for search of depressed teens. Controls were those who did not have these codes.
Exclusion criteria: Charts that did not contain the following study data were not included: Subject demographics (age, race, sex), subject vital signs- heart rate, blood pressure, height/weight, BMI, concurrent diagnoses (medical and psychiatric).
A two-way type III ANOVA using normal scores transformed variables was used to analyze systolic and diastolic BP percentiles and pulse rates as dependent variables and sex (male/female), and depression status (depressed/non-depressed) entered as fixed factors. Transforming all data to normal quantiles or normal scores makes the tests nonparametric and less sensitive to any existing outliers in the data that may affect the outcomes.
Results
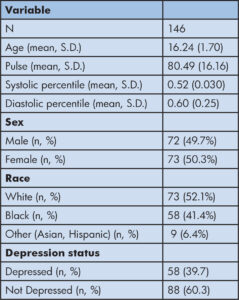
There were 146 patients, 58 (39.7%) with depression and 88 (60.3%) without the depression diagnosis (control group). There were equal numbers of male and female patients with a mean age of 16.2 years (Table 1).
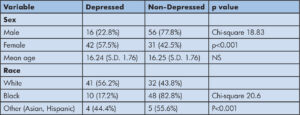
In our study population, there were 16 (22.8%) of male adolescents vs. 42 (57.5%) of female adolescents categorized as depressed (Chi-square 18.83, p <0.001); mean age was the same for depressed adolescents vs. not depressed at 16.2 years and 44 (55.7%) of white adolescents, 10 (17.2%) of black adolescents and 4 (44.4%) of other (Asian, Hispanic, other) were in the depressed category (Chi-square 20.6, p<0.001) (Table 2).
On two-way type III ANOVA using transformed variables, there were significantly higher systolic blood pressure percentiles in depressed patients vs. non-depressed (57.4 vs. 47.8; F (DF 1) = 4.48, p = .030. There was no main effect of depression on diastolic blood pressure and there was no interaction effect of sex and depression (Table 3).
Table 3: Comparison of Mean BP percentiles: Non-Depressed vs. Depressed (Two-way type III ANOVA). No significant interaction effect between Depression and Sex.
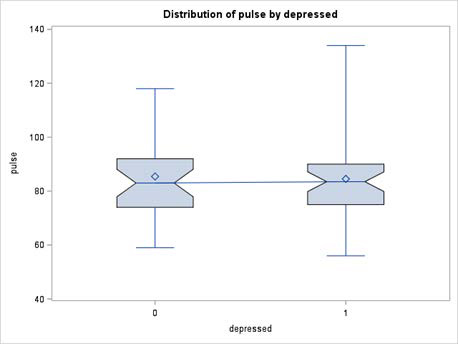
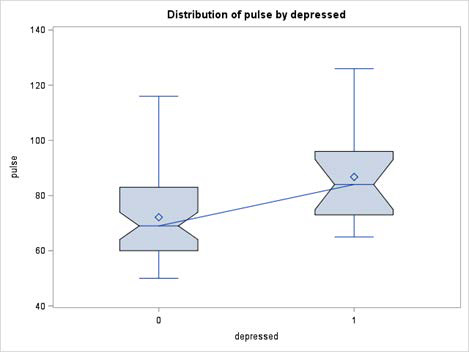
Finally, there was a significant interaction effect of depression and sex on pulse rate so that higher mean Pulse Rates were found in depression only among males but not females. (males depressed mean PR was 86.7 vs. males non-depressed PR of 72.1; F (DF 1) = 8.61, p =.003) (Figure 1a and Figure 1b). The statistical power (of the interaction test sex by depressed) for the only significant variable pulse, was found to be 85% using G*power.
A separate analysis was conducted addressing the potential influence of obesity and race on HR and BP percentiles and were not found to be statistically different between depressed vs. non-depressed groups.
Discussion
Studies investigating the association between BP and depression have had inconsistent results ranging from a positive association18, a negative association19, or even a nonexistent association.24
In this study, significantly higher systolic blood pressure percentiles were found in depressed patients vs. non-depressed with no significant effect of depression on diastolic blood pressure. Our findings are in accordance with data from the British Whitehall II Study, suggesting that the risk of hypertension increased with repeated experience of depressive symptoms over time.7 The strength of that study includes the use of five waves of screening data of depressive symptoms and blood pressure, however, the patients’ ages ranged from 35 to 55 at baseline, and the findings were not significant in women.25
One of the proposed mechanisms for the association between hypertension and psychopathology is genetic susceptibility. It is widely accepted that genetics plays a significant role in the susceptibility to hypertension.26 It is also suggested that genetic factors play an important role in the pathophysiology of mood disorders.27
Other studies did not find the association between higher BP in depressed patients. Hildrum et al., found BP was lower in patients with depression.28 This finding was supported by subsequent longitudinal research (HUNT study) on the same population, even when those on medications for depression or hypertension were excluded.19 Of the proposed mechanisms to explain this association is a causative role for hypotension in the pathogenesis of depression through somatic symptoms and fatigue. A physiologic explanation for this association is that the central monoamine system may mediate hypotension and depression. In this system, altered levels of neuropeptide Y are thought to suppress sympathetic activity leading to a decrease in BP with depression.29
Such results are intriguing and contradict the hypothesis that hypertension plays a role in the association between psychopathology and CVD as mentioned earlier.17 These disparate findings are unexplained, but may involve differences in study populations. For example, comparing the HUNT study to the Whitehall study, the latter had a much higher proportion of nonwhite participants in which they reported higher odds for hypertension.19 Conflicting results could also be due to the different ways of defining hypertension as some studies have used self-reported hypertension instead of measuring blood pressure30, short periods of follow up20, different age groups studied30, or not accounting for confounding factors such as the use of antidepressants.20
Few studies pertain to adolescents. One of these is the Western Australian Pregnancy Cohort (Raine) Study, where an inverse association between depression and blood pressure was found in 14-year-old boys.22 This is in agreement with another prospective 20-year cohort study.21 To add to the confusion, Hammerton and coworkers31 found that lower systolic blood pressure could predict new-onset depressive disorders in high-risk children (offspring of mothers experiencing recurrent depression), but they also found that adolescents from the general population with higher blood pressure showed a higher risk of development of future depressive disorders.
Differences between studies could be explained by the differences in the study populations, population age, antidepressant or antihypertensive treatment, different means of assessing depression, and blood pressure recording methods. In our study, a significantly higher pulse rate was found in depressed males but not depressed female adolescents. This is a novel finding. A high heart rate has been associated with an increased risk of future CVD in the general population32 and is also found in patients with established CVD.33 It is hypothesized but still unclear whether the increased resting pulse rate plays a role in the association between CVD and psychopathology.34 Our results are in accordance with the FINE study where higher heart rate was found to correlate with depression in elderly men but was found not to cause subsequent cardiac events.34 However, the HUNT study reported only a weak cross-sectional association between depression and increased pulse rate.19 It is likely that complex interactions of environmental stressors and resulting physiologic responses may mediate this phenomenon.
The strengths of the current study included the study of adolescents which is an age that has not been well studied regarding depression and physiologic parameters. Blood pressure percentiles for age, height, and sex were used which is a more valid variable for analysis. The diagnosis of depression in this study was made by one board certified Adolescent Medicine subspecialist adding consistency and is derived from clinical data. The significantly higher depression rates among females versus males and in white versus other races (Table 2) in our clinic sample, represents the nature of our clinic and the population that it serves.
There are limitations of this study including the retrospective, case-control study design, and measuring data at one point in time with no long-term follow up. This is a preliminary study in a small group of patients attending an adolescent clinic.
Also, data to control for potential confounding variables known to cause secondary hypertension or elevated PR in children such as renal disease, cardiac disease, endocrine disorders, and certain medications was not included in the analysis nor was family history of hypertension included. Also, the reason for this visit was not included as a potential confounding variable. Other limitations are that this study was conducted in a single clinic which limits generalizability and that BP was measured with a single automated sphygmomanometer measurement and not a continuous ambulatory method.
Conclusion
Significantly higher systolic blood pressure percentiles were found in depressed vs. non-depressed adolescents. Pulse rates were higher in males who were depressed vs. non-depressed but this relationship was not seen in females. Future expanded study of these findings is warranted.
References
- Tiemeier H, van Dijck W, Hofman A, Witteman JC, Stijnen T, Breteler MM. Relationship between atherosclerosis and late-life depression: the Rotterdam Study. Arch Gen Psychiatry. 2004;61(4):369-376.
- Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Roose SP, Sheps DS. Consensus statement on depression, anxiety, and cardiovascular disease. J Clin Psychiatry. 2001;62 Suppl 8:24-27.
- Masters KS, Shaffer JA, Vagnini KM. The Impact of Psychological Functioning on Cardiovascular Disease. Curr Atheroscler Rep. 2020;22(10):51.
- Bordoni B, Marelli F, Morabito B, Sacconi B. Depression and anxiety in patients with chronic heart failure. Future Cardiol. 2018;14(2):115-119.
- Cohen BE, Edmondson D, Kronish IM. State of the Art Review: Depression, Stress, Anxiety, and Cardiovascular Disease. Am J Hypertens. 2015;28(11):1295-1302.
- Hare DL, Toukhsati SR, Johansson P, Jaarsma T. Depression and cardiovascular disease: a clinical review. Eur Heart J. 2014;35(21):1365-1372.
- Penninx BW. Depression and cardiovascular disease: Epidemiological evidence on their linking mechanisms. Neurosci Biobehav Rev. 2017;74(Pt B):277-286.
- Seldenrijk A, Vogelzangs N, Batelaan NM, Wieman I, van Schaik DJ, Penninx BJ. Depression, anxiety and 6-year risk of cardiovascular disease. J Psychosom Res. 2015;78(2):123-129.
- Barth J, Schumacher M, Herrmann-Lingen C. Depression as a risk factor for mortality in patients with coronary heart disease: a meta-analysis. Psychosom Med. 2004;66(6):802-813.
- Silverman AL, Herzog AA, Silverman DI. Hearts and Minds: Stress, Anxiety, and Depression: Unsung Risk Factors for Cardiovascular Disease. Cardiol Rev. 2019;27(4):202-207.
- Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, Raghuveer G, et al. Major Depressive Disorder and Bipolar Disorder Predispose Youth to Accelerated Atherosclerosis and Early Cardiovascular Disease: A Scientific Statement From the American Heart Association. Circulation. 2015;132(10):965-986.
- Palta P, Samuel LJ, Miller ER, Szanton SL. Depression and oxidative stress: results from a meta-analysis of observational studies. Psychosom Med. 2014;76(1):12-19.
- Miller GE, Cole SW. Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biol Psychiatry. 2012;72(1):34-40.
- Ryder JR, O’Connell M, Bosch TA, Chow L, Rudser KD, Dengel DR, et al. Impaired cardiac autonomic nervous system function is associated with pediatric hypertension independent of adiposity. Pediatr Res. 2016;79(1-1):49-54.
- Stokes J, Kannel WB, Wolf PA, D’Agostino RB, Cupples LA. Blood pressure as a risk factor for cardiovascular disease. The Framingham Study–30 years of follow-up. Hypertension. 1989;13(5 Suppl):I13-18.
- Carroll D, Smith GD, Shipley MJ, Steptoe A, Brunner EJ, Marmot MG. Blood pressure reactions to acute psychological stress and future blood pressure status: a 10-year follow-up of men in the Whitehall II study. Psychosom Med. 2001;63(5):737-743.
- Scuteri A. Depression and cardiovascular risk: does blood pressure play a role? J Hypertens. 2008;26(9):1738-1739.
- Jani BD, Cavanagh J, Barry SJ, Der G, Sattar N, Mair FS. Relationship Between Blood Pressure Values, Depressive Symptoms, and Cardiovascular Outcomes in Patients With Cardiometabolic Disease. J Clin Hypertens (Greenwich). 2016;18(10):1027-1035.
- Hildrum B, Romild U, Holmen J. Anxiety and depression lowers blood pressure: 22-year follow-up of the population based HUNT study, Norway. BMC Public Health. 2011;11:601.
- Delaney JA, Oddson BE, Kramer H, Shea S, Psaty BM, McClelland RL. Baseline depressive symptoms are not associated with clinically important levels of incident hypertension during two years of follow-up: the multi-ethnic study of atherosclerosis. Hypertension. 2010;55(2):408-414.
- Bhat SK, Beilin LJ, Robinson M, Burrows S, Mori TA. Relationships between depression and anxiety symptoms scores and blood pressure in young adults. J Hypertens. 2017;35(10):1983-1991.
- Louise S, Warrington NM, McCaskie PA, Oddy WH, Zubrick SR, Hands B, et al. Associations between anxious-depressed symptoms and cardiovascular risk factors in a longitudinal childhood study. Prev Med. 2012;54(5):345-350.
- Shah MT, Zonderman AB, Waldstein SR. Sex and age differences in the relation of depressive symptoms with blood pressure. Am J Hypertens. 2013;26(12):1413-1420.
- Grimsrud A, Stein DJ, Seedat S, Williams D, Myer L. The association between hypertension and depression and anxiety disorders: results from a nationally-representative sample of South African adults. PLoS One. 2009;4(5):e5552.
- Nabi H, Chastang JF, Lefèvre T, Dugravot A, Melchior M, Marmot MG, et al. Trajectories of depressive episodes and hypertension over 24 years: the Whitehall II prospective cohort study. Hypertension. 2011;57(4):710-716.
- Grewen KM, Girdler SS, Hinderliter A, Light KC. Depressive symptoms are related to higher ambulatory blood pressure in people with a family history of hypertension. Psychosom Med. 2004;66(1):9-16.
- Nurnberger JI, McInnis M, Reich W, Kastelic E, Wilcox HC, Glowinski A, et al. A high-risk study of bipolar disorder. Childhood clinical phenotypes as precursors of major mood disorders. Arch Gen Psychiatry. 2011;68(10):1012-1020.
- Hildrum B, Mykletun A, Stordal E, Bjelland I, Dahl AA, Holmen J. Association of low blood pressure with anxiety and depression: the Nord-Trøndelag Health Study. J Epidemiol Community Health. 2007;61(1):53-58.
- Head GA. Central monoamine neurons and cardiovascular control. Kidney Int Suppl. 1992;37:S8-13.
- Gangwisch JE, Malaspina D, Posner K, Babiss LA, Heymsfield SB, Turner JB, et al. Insomnia and sleep duration as mediators of the relationship between depression and hypertension incidence. Am J Hypertens. 2010;23(1):62-69.
- Hammerton G, Harold G, Thapar A. Depression and blood pressure in high-risk children and adolescents: an investigation using two longitudinal cohorts. BMJ Open. 2013;3(9):e003206.
- Tverdal A, Hjellvik V, Selmer R. Heart rate and mortality from cardiovascular causes: a 12 year follow-up study of 379,843 men and women aged 40-45 years. Eur Heart J. 2008;29(22):2772-2781.
- Fox K, Ford I, Steg PG, Tendera M, Robertson M, Ferrari R, et al. Heart rate as a prognostic risk factor in patients with coronary artery disease and left-ventricular systolic dysfunction (BEAUTIFUL): a subgroup analysis of a randomised controlled trial. Lancet. 2008;372(9641):817-821.
- Kamphuis MH, Geerlings MI, Dekker JM, Giampaoli S, Nissinen A, Grobbee DE, et al. Autonomic dysfunction: a link between depression and cardiovascular mortality? The FINE Study. Eur J Cardiovasc Prev Rehabil. 2007;14(6):796-802.