Red Eye: An Unusual Suspect
AUTHORS:
Anusha S. Tuli1; Alexander H. Dang2; Ruchita Kachru, MD3; Ankit Shah, MD4
1Barnard College, Columbia University, New York, New York
2Harvard University, Cambridge, Massachusetts
3Department of Pediatrics, University of Florida, Gainesville, Florida
4Department of Ophthalmology, University of Florida, Gainesville, Florida
STUDENT ARTICLE | PUBLISHED SPRING 2023 | Volume 43, Issue 2
DOWNLOAD PDF
Introduction
Red eye is common in children and is often associated with viral or allergic conjunctivitis. In these cases, the condition is usually bilateral and associated with tearing. The list of other conditions leading to red eye is long and includes infectious, inflammatory, autoimmune, and traumatic causes. Herpes simplex keratitis (HSK) is one of the more common infectious causes of red eye in children but usually presents as unilateral blepharoconjunctivitis with eyelid vesicles and a follicular conjunctivitis. Corneal involvement in childhood is rare as it is usually associated with recurrent disease that occurs in adulthood. The classic dogma is that herpes simplex virus (HSV) type 1 causes infections above the waistline while HSV type 2 (HSV-2) causes genital herpes as well as congenital herpes as the neonate gets infected passing through the infected birth canal. Here we present a case report of a young girl with a corneal ulcer caused by HSV-2.
Case Report
An 11-year-old female was referred to the emergency department (ED) by an optometrist as they were concerned about a corneal ulcer in her right eye. Approximately three weeks prior to presentation, the patient had developed a foreign body sensation in her right eye associated with some redness. Her mother assumed she had pink eye and had started over the counter lubricating drops as well as “pink eye” drops without improvement. Subsequently, the patient noted blurry vision in that eye that appeared to be worsening, so she went to an optometrist who prescribed moxifloxacin and prednisolone acetate eye drops. She was then sent to a second optometrist who was concerned about a corneal ulcer and sent her to the ED.
On presentation to the ED, the patient complained that she had persistent foreign body sensation in the right eye associated with redness, irritation, and decreased vision. She denied contact lens wear but did wear glasses for vision correction for astigmatism and refractive error. There was no history of trauma or other eye problems in the past. Her past medical history was only positive for attention deficit hyperactivity disorder and asthma and negative for fever blisters. She had no allergies and review of systems was completely negative. She was in school, denied being sexually active, and lived with her mother, older sister, and the sister’s boyfriend.
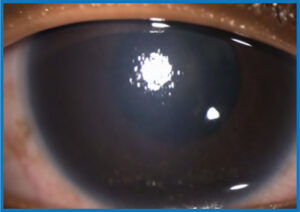
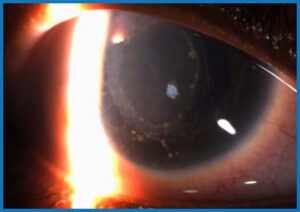
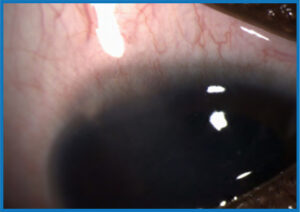
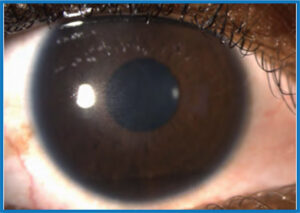
On examination, she appeared healthy and well-nourished and the only pertinent abnormal findings were in the right eye. The vision in the right eye was hand motions only, while the left eye was 20/25. Intraocular pressure was slightly decreased in the right eye at 16 mm Hg compared to 23 in the left eye. Pupils, extraocular movements, and external ocular examination were normal with no rash on the eyelids. On slit lamp examination of the right eye, she was noted to have a protective ptosis, follicular conjunctivitis and diffuse haze of the cornea (Figure 1). There were granulomatous keratic precipitates in a ring fashion on endothelium (Figure 2), limbal elevation superiorly (Figure 3), and a small dendritiform lesion centrally. The anterior chamber could not be viewed due to the corneal haze but the lens appeared clear. There was no view of the fundus due to media haziness. The left eye was completely within normal limits.
Given the findings, the initial differential diagnoses considered were anterior uveitis from sarcoid, tuberculosis, syphilis, or Lyme disease or herpes simplex or zoster keratitis. Conjunctival swabs for PCR for herpes simplex virus (HSV) and varicella VZV and a chest X-ray were obtained and blood was drawn for laboratory testing including CBC with differential, HLA-B27, rheumatoid factor, C-reactive protein, erythrocyte sedimentation rate, syphilis tests, Lyme antibodies, Lysozyme, ACE, ANCA, ANA, and QuantiFERON-TB Gold. The patient was started on valacyclovir 1 gm TID orally and cyclopentolate 1% TID topically OD due to the high suspicion for a herpetic keraitis. The steroid and antibiotic eye drops were continued.
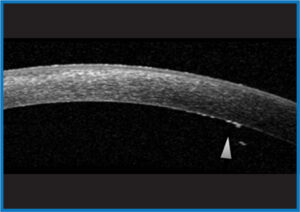
The patient was seen in the eye clinic the next day with an unchanged exam other than resolution of the corneal dendrite. The PCR test for HSV-2 was noted to be the only positive test at this time. The corneal sensation was tested in the right eye during this visit and was found to be diminished compared to the left eye. A B-scan ultrasound was performed to evaluate the posterior chamber and was found to be normal with no evidence of inflammation. An anterior segment ocular coherent tomography was performed and confirmed the keratic precipitates on the endothelium (Figure 4, arrow). Patient was continued on valacylovir and the prednisolone acetate was increased to every 2 hours while awake. Cyclopentolate was continued and moxifloxacin was discontinued.
A long discussion with patient and mother was undertaken as HSV-2 infection is usually sexually transmitted. Patient denied being sexually active or being abused. However, given the age of the patient, the department of child protection services was consulted who did not find any evidence of abuse. It was therefore assumed that she had likely contracted HSV-2 during birth and this had stayed latent in her trigeminal ganglion and recurred at this time.
Patient returned one week later and indicated that she was doing much better. Vision had improved to 20/100 with decrease in the keratic precipitates and corneal edema. The medications were continued. Six weeks following the initial visit, the vision had improved to 20/25 with faint pigmented keratic precipitates on the endothelium and mild corneal haze (Figure 5). The valacyclovir was decreased to 500 mg daily and the prednisolone was tapered gradually to one drop on alternate days over the next 4 months. However, at that dose, the patient’s vision declined to 20/100 and it was noted that she had increased inflammation and corneal edema. The prednisolone was increased to twice a day for a month and then decreased back to once a day after another month (when the eye was noted to be quiet again) with plans to continue that treatment long-term along with valcyclovir 500 mg daily long-term to prevent recurrences.
Discussion
Herpes simplex is a double stranded DNA virus that belongs to the Herpesviridae family, which includes other members such as herpes zoster virus and cytomegalovirus.1 Common to all the members of the family is the condition of latency where the virus, upon entering the body, resides in either the nervous or hemolymphatic system permanently in a quiescent state.2 A change in the immunological status of the host results in reactivation of the virus (lytic phase), causing recurrent disease.3 In some cases, such as in herpes zoster virus, reactivation usually results in immunity for a period, during which the virus becomes latent again. However, in the case of herpes simplex virus, reactivation occurs frequently, and although the virus becomes latent between reactivations, the recurrence rate increases with increased number of recurrences.4
Herpes simplex has two members: HSV type -1, which usually resides latent in the trigeminal ganglion most commonly causes oral, nasal, and ocular disease and HSV-2, which usually lies dormant in the sacral ganglia, commonly causes genital herpes and is often spread through sexual activity.4 HSV-2 affects the eyes less frequently than HSV-1 and is thought to cause more severe disease. It is unknown whether ocular disease with HSV-2 is caused by direct contact of the ocular mucus membranes with infected secretions from the sexual partner, or whether it is due to self-inoculation from genital herpes. HSV-2 may also be transmitted to babies as they pass through the birth canal of infected mothers, and this is the most likely method of infection in this child. Research has shown that latently infected individuals asymptomatically shed the virus in their secretions frequently, and that this is the primary mode of transmission.5
Unilateral blepharoconjunctivitis characterized by a vesicular dermatitis of the eyelids with an associated follicular conjunctivitis is the most common ocular manifestation of HSV in children.6 This presentation is commonly misdiagnosed as impetigo, “pink eye,” staphylococcus blepharitis, or phylectenular Keratoconjunctivitis especially if the cutaneous lesions are sparse and overlooked. These lesions usually resolve spontaneously without sequelae. Subsequent recurrent disease can manifest as blepharoconjunctivitis, but more frequently seen as infection of the cornea known as keratitis. Unlike adults, both recurrent disease and bilateral disease is much more common in children especially if the child has a history of atopic disease and asthma.7
HSV keratitis can be subdivided into epithelial, stromal, and endothelial, though multiple layers of the cornea may be affected at the same time.
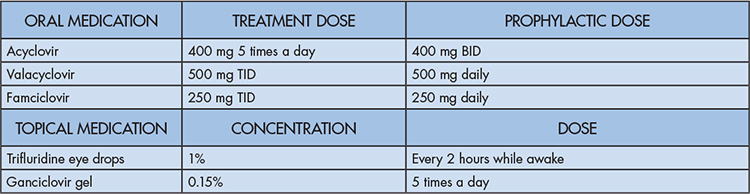
- Epithelial keratitis: The prototypical lesion is a dendrite (branching lesion), on the corneal surface. Dendrites classically have dichotomous branches and terminal bulbs at the end of each branch (Figure 6). The virally infected cells are at the border of the dendrite with an epithelial defect centrally.8 Occasionally, in immunocompromised individuals, or those on topical steroids, the lesion enlarges and becomes a geographic ulcer.8 These lesions usually take longer to resolve with treatment and can have underlying inflammation. Epithelial disease is treated with either oral or topical antiviral medication with adjunct surgical debridement. (Table 1).9
- Stromal keratitis: This is usually differentiated into two types: with and without necrosis. Stromal disease without necrosis is thought to be a host immunological response to viral antigen in the cornea rather than to live virus. It is manifested by patchy inflammation in the corneal stroma (interstitial keratitis) without involvement of the epithelium or endothelium.10 When treated early, it resolves completely without residual scarring. However, untreated interstitial keratitis can lead to permanent corneal vascularization that can affect the vision and lead to lipid keratopathy due to serum leaking out of these vessels.11 Lipid keratopathy is one of the major causes of vision loss from HSV keratitis. Unfortunately, the corneal scarring and opacification usually associated with untreated stromal keratitis in young (less than 8-years-old) pediatric patients can have devastating impact on vision as it predisposes these patients to deprivational and astigmatic amblyopia.12 Stromal disease with necrosis (necrotizing keratitis) is thought to occur in patients that have had several bouts of recurrent disease in which there is an immune response to viral antigen deposited from previous bouts of HSV in addition to live virus.13 This can lead to severe inflammation in the cornea and ulceration that can cause the cornea to perforate. This needs to be treated urgently with oral antivirals as well as steroids but often has poor outcomes due to residual scarring and corneal thinning.14
- Endotheliitis (disciform keratitis): This is an inflammatory response to viral antigen or live virus in the endothelial layer of the cornea, and can be described as disciform, diffuse or linear based on its appearance.15 The endothelium cells function by dehydrating the cornea to maintain its clarity. Any insult to the endothelial cell function (through inflammation or infection) results in swelling and thickening of the cornea. The inflammation associated with HSV endotheliitis presents as granulomatous keratic precipitates, translucent spots of inflammation usually in a ring shape on the inner layer of the cornea.16 Early treatment with topical steroids is crucial in treating this condition, reducing corneal edema, and preventing permanent vision loss.17
Conclusion
This patient had a combination of follicular conjunctivitis and endotheliitis, which is an unusual presentation. Therefore, she was treated with therapeutic doses of valacyclovir as well as high doses of steroids to treat the infectious and inflammatory components, with an excellent outcome. Given the severity of the initial episode, the plan was to keep her on a prophylactic dose of valacyclovir long-term. Although we attempted to taper off her steroids gradually, she had recurrence of her inflammation upon decreasing it to alternate days. This is likely because there is persistent viral antigen in the endothelium and she will require a low dose of topical steroids long-term to prevent her inflammation from flaring up. Unfortunately, even prophylactic antivirals do not eliminate the risk of recurrence, and she is at high risk to have additional episodes.18 She and her mother were therefore counseled that she would need frequent eye exams and that they should return immediately if she developed a red eye in the future.
References
- Rechenchoski DZ, Faccin-Galhardi LC, Linhares REC, et al. Herpesvirus: an underestimated virus. Folia Microbiol (Praha). 2017;62(2):151-156. doi: 10.1007/s12223-016-0482-7. Epub 2016 Nov 17. Erratum in: Folia Microbiol (Praha). 2017 Jul 28;: PMID: 27858281.
- Preciado-Delgadillo, M, Lorenzo-Mejía, A, Hitos-Fajer, A. Arellanes-García, L. (). Herpetic Keratouveitis in Children. International Ophthalmology Clinics. 2008;48 (3):39-49. doi: 10.1097/IIO.0b013e31817d9876
- Lan K, Luo MH. Herpesviruses: epidemiology, pathogenesis, and interventions. Virol Sin. 2017, 32(5):347-348. doi: 10.1007/s12250-017-4108-2. PMID: 29116595; PMCID: PMC6598912.
- Harris, K. (). Herpes Simplex Virus Keratitis. Home Healthcare Now. 2019;37 (5):281-284. doi: 10.1097/NHH.0000000000000791.
- Sawtell NM, Thompson RL. Alphaherpesvirus latency and reactivation with a focus on herpes simplex virus. Curr Issues Mol Biol. 2021;41:267-356. doi: 10.21775/cimb.041.267. Epub 2020 Sep 4. PMID: 32883886.
- Revere K., Davidson SL. Update on management of herpes keratitis in children. Current Opinion in Ophthalmology, 2013;24 (4), 343-347. doi: 10.1097/ICU.0b013e32836227d8
- Liu S, Pavan-Langston D, Colby KA. (). Pediatric herpes simplex of the anterior segment: characteristics, treatment, and outcomes. Ophthalmology. 2012;119 (10):2003-2008
- Hill GM, Ku ES, Dwarakanathan S. Herpes simplex keratitis. Dis Mon. 2014;60(6):239-46. doi: 10.1016/j.disamonth.2014.03.003. PMID: 24906668.
- Njoya JM, Handor H, Lezrek O, et al. Herpetic epithelial keratitis. QJM. 2015;108(7):595. doi: 10.1093/qjmed/hcu250. Epub 2014 Dec 17. PMID: 25524905
- Rowe AM, St Leger AJ, Jeon S, et al. Herpes keratitis. Prog Retin Eye Res. 2013;32:88-101. doi: 10.1016/j.preteyeres.2012.08.002. Epub 2012 Aug 27. PMID: 22944008; PMCID: PMC3529813
- Biswas PS, Rouse BT. Early events in HSV keratitis–setting the stage for a blinding disease. Microbes Infect. 2005;7(4):799-810. doi: 10.1016/j.micinf.2005.03.003. Epub 2005 Mar 22. PMID: 15857807.
- Hsiao, C., Yeung L, Yeh L, Kao L, et al. (). Pediatric herpes simplex virus keratitis. Cornea, 2009;28 (3), 249-253. doi: 10.1097/ICO.0b013e3181839aee
- Rowe AM, St Leger AJ, Jeon S, et al. Herpes keratitis. Prog Retin Eye Res. 2013;32:88-101. doi: 10.1016/j.preteyeres.2012.08.002. Epub 2012 Aug 27. PMID: 22944008; PMCID: PMC3529813
- Bourne WM. Corneal endothelium–past, present, and future. Eye Contact Lens. 2010;36(5):310-4. doi: 10.1097/ICL.0b013e3181ee1450. PMID: 20724858.
- Tsatsos M, MacGregor C, Athanasiadis I, et al. Herpes simplex virus keratitis: an update of the pathogenesis and current treatment with oral and topical antiviral agents. Clin Exp Ophthalmol. 2016;44(9):824-837. doi: 10.1111/ceo.12785. Epub 2016 Jul 26. PMID: 27273328.
- Kabra A, Lalitha P, Mahadevan K, et al. Herpes simplex keratitis and visual impairment: a case series. Indian J Ophthalmol. 2006;54(1):23-7. doi: 10.4103/0301-4738.21610. PMID: 16531666.
- Vadoothker S, Andrews L, Jeng B, Levin M. Management of herpes simplex virus keratitis in the pediatric population. The Pediatric Infectious Disease Journal, 2018;37 (9), 949-951. doi: 10.1097/INF.0000000000002114.
- Herpetic Eye Disease Study Group. Acyclovir for the prevention of recurrent herpes simplex virus eye disease. N Engl J Med. 1998;339:300–6.