Recommendations on Teen Depression for the Primary Care Provider
AUTHOR:
Jasmine M Reese, MD MPH FAAP FSAHM
Johns Hopkins School of Medicine, Johns Hopkins All Children’s Hospital
Review Article | PUBLISHED SPRING 2023 | Volume 43, Issue 2
DOWNLOAD PDF
“I thought my pediatrician was the wrong person to talk to about my depression”. This is a statement made by a 14-year-old adolescent that was seeking help from her pediatrician regarding changes in her mood and was discharged from clinic before any discussion or evaluation took place. It is “old thinking” to say that when a pediatric patient has concerns about feeling depressed that they should only be seen by a psychiatrist or a psychologist. The unfortunate reality is that many teens are struggling with mood changes, including depression. Pediatricians are the front-line providers to help them navigate first steps in screening, diagnosis, and initial management.
According to the National Institute of Mental Health, approximately 4.1 million adolescents ages 12-17 years had at least one episode of major depression. The prevalence of Major Depressive Disorder (MDD) in children and adolescents is approximately 2% and 13%, respectively. Adolescent females tend to have higher rates of depression when compared to males.5 The lifetime prevalence is 20% by age 20 years old.17 According to the National Youth Risk Behavior Survey there has been an upward trend in high school students experiencing persistent feelings of sadness or hopelessness, who have considered attempting suicide, and who made a suicide plan.3
As medical students, physicians may recall learning about the specific details regarding rare and complex pediatric disease processes including heart disease, congenital malformations, respiratory illnesses, diabetes, and many others. However, physicians may not recall learning the top 3 leading causes of death among the adolescent and young adult age group which include unintentional injuries, suicide, and homicide.10 With suicide as the second leading cause of death among teens, it would behoove the general pediatrician to understand how to best approach mental health concerns in this population.
According to a recent national poll of parents of adolescents ages 11-18 years, primary care providers (PCPs) ask their child about mental health concerns during 41% of their check-up visits. Fourteen percent of parents reported their child is never asked about mental health. Sixteen percent of parents reported that their teens would definitely talk to their PCPs about their mental health and 57% thought their teens would probably discuss this with their PCP.13 This parent perspective may be helpful for providers in understanding that they are the front-lines in identifying adolescent mental health needs.
When reviewing rates of depression encountered in the primary care setting, 2 in 3 adolescents with depression are missed by PCPs and do not receive the necessary care. Of those that are identified, only half receive the right kind of care and there is often a gap in completion rates of mental health referrals.17
When screening adolescents for depression, pediatricians should consider the individual’s risk. Many factors can play a role in the development of depression including biologic, environmental, psychologic, and genetic. Many teens are challenged with many stressors including loss, abuse, and neglect. Those struggling with chronic medical illness such as diabetes, asthma, obesity, and epilepsy are also at increased risk. Additionally, family history of depression should be considered as well as other history of co-existing mental health disorders including anxiety, ADHD, substance use, and eating disorders.5
An additional risk factor that pediatricians should take into consideration is one that is truly universal to all individuals—the COVID-19 pandemic. There is a growing body of literature highlighting the negative impact that the pandemic has had on the mental and physical health of many youth. Studies including parent surveys across the U.S. showed that both teen girls and teen boys were noticed to have new or worsening anxiety, depression, sleep issues, withdrawing from families, and aggressive behavior during the pandemic.11 In another adolescent self-report study of over 700 adolescents, mental health was reported as one of their top three challenges during the COVID-19 pandemic.14
Over the years there has been more awareness regarding the use of social media among adolescents, and pediatricians are encouraged to ask about child and teen social media use. 93-97% of 13-17-year-old adolescents use at least one social media platform and are likely spending more than 3 hours per day on social media.16 There are also reports of increased number of teens experiencing cyberbullying especially after the reliance on virtual school and virtual social networks since the pandemic started.2,7
The AAP and the USPSTF recommend that pediatricians screen adolescents for depression in youth 12 years and over during their annual care visits and have a plan for management when depression is identified.6 There are many reasons why this may pose a challenge especially in a busy clinical practice setting including scope of training, experience and time. There are several resources that exist and are supported by the AAP that provide guidance for the general pediatrician. In 2018, the GLAD-PC Guidelines were updated to include evidence-based practices that are both feasible and optimal for addressing child and adolescent mental health in a primary care setting.4,17
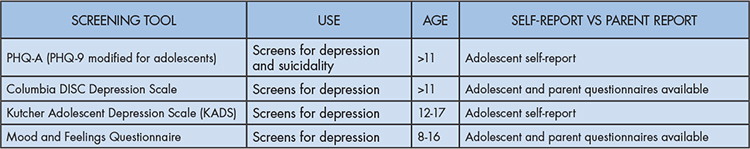
Primary care providers should screen for depression in teens who present with a chief complaint concerning for a mental health concern or emotional problem, high score on a screening tool, and who are considered to be at high-risk. There are several screening tools that exist and providers should aim to use screening tools that are validated, brief, free and feasible to implement into their clinical work-flow. Specifically, for adolescent depression, brief screening tools to consider include the Patient Health Questionnaire-9 modified for adolescents (PHQ-A) or Columbia DISC Depression Scale (Table 1). Other validated screening tools do exist, however may be longer and/or require payment for use.17
Before a diagnosis can be made, providers should consider their differential diagnosis as there can be many overlapping symptoms among depression and other medical illnesses. Other medical causes for symptoms such as sleep difficulty, low energy, fatigue, agitation, or mood changes can be attributed to problems such as thyroid dysfunction, anemia, vitamin deficiency, malnutrition, sleep apnea, substance use/abuse. Rarely, other causes can include more chronic and severe illnesses such as autoimmune disorders, vascular disease, hematologic disease, neurologic illness, and inherited disorders. Thorough history is extremely important in order to tease out whether the patient requires a more extensive evaluation for something other than a mental health diagnosis. Equally as important is taking time to talk alone with the adolescent patient. This one-on-one time may give the provider more insight as to concerning behaviors or symptoms that the teen does not feel comfortable expressing in front of their parent or caregiver.
The general pediatrician should become familiar with use of the DSM-5 when making a diagnosis of Major Depressive Disorder (MDD). Symptoms and timeframe are important in making this diagnosis (Table 2). The adolescent should have 5 or more symptoms in a 2-week period and at least one symptom should be depressed mood or loss of interest/pleasure. Other symptoms should be consistent with appetite or weight change, sleep disturbance, slowing down or restlessness, loss of energy, worthlessness or guilt, difficulty concentrating, and recurrent thoughts of death or suicidal ideation. The adolescent may not report each of these symptoms or may not meet the time frame for MDD and the provider may consider other diagnoses such as Persistent Depressive Disorder (PDD). Criteria for PDD include depressed mood or irritability for the majority of days in a 1-year period.1
Once the diagnosis of MDD is confirmed, it is important to categorize the severity of the depression in order optimize the treatment and management plan. History and risk factors are most important in understanding severity of illness however, screening tool scores can be helpful. For example, a PHQ-9 score of 5-9 is most consistent with mild depression; PHQ-9 score of 10-14 is most consistent with moderate depression; and PHQ-9 score of 20 is most consistent with severe depression.17,12 It is important not to rely solely on screening tool scores because screening tools are not diagnostic. The severity of illness is also best approached by understanding the individual’s level of daily functioning. For example, if the teen is able to excel in most areas such as academics, activities, family/peer relationships, then they are likely to be classified as having mild depression. For a teen who has very limited functioning or daily disruption including failing grades, loss of engagement in activities or loss of relationships they are most likely categorized as moderate to severe depression.
Treatment and management of adolescent depression should be based on the severity of the depression. For a teen with mild depression, active monitoring by the general pediatrician is a good initial step. Active monitoring includes frequent or routine check-in visits with the patient to ensure symptoms have not worsened.4 The provider should use their clinical judgement to develop the best approach for active monitoring that is feasible for the patient, family, and for themselves as the provider. For example, using a sick-visit appointment time 2 weeks after the initial diagnosis of depression was made may be used as a brief follow-up appointment where the focus would be on addressing any mood changes or mental health concerns. Scheduling a telemedicine appointment for these types of visits can also be considered. For adolescents with more moderate or severe symptoms, one should consider and discuss the benefits of both routine therapy as well as initiating a psychotropic medication. Active monitoring by the pediatrician should still take place, however, a therapist or counselor who can provide evidence-based therapy, including cognitive behavioral therapy (CBT), should be considered as part of the management plan.4
Discussing therapy and psychotropic medications may feel unfamiliar and/or uncomfortable for many general pediatricians. This is why not only reviewing the mental health resources, such as the AAP mental health toolkit or the GLAD-PC guidelines in advance is important but also where practice makes perfect!…or at least makes for a more confident provider!
Evidence-based approaches for psychotherapy for adolescent depression include CBT and interpersonal psychotherapy (IPT).4 Providers should aim to be familiar with the local resources and what types of therapy are offered either within their medical organization or within their local community. In the same way, it may be helpful to know which insurance plans therapists are in network with and who offers telemedicine appointments.
In choosing a psychotropic medication, providers should have knowledge of which psychotropic medications are FDA approved for the adolescent age group as well as the common side effect profile so they can provide appropriate anticipatory guidance to patients and families. Common side effects include headache, nausea, feeling tired, agitation, sleep and appetite changes. Typically, negative side effects occur early on after starting the medication and may go away after several days.9 There are limited studies on child and adolescent psychotropic medication efficacy. The Treatment for Adolescents with Depression Study (TADS) is often referenced as the best gauge on medication efficacy. Currently, two SSRIs are FDA approved for this age group and include Fluoxetine for ages 8-18 years of age and Escitalopram for ages 12-17.4 Although there are many other SSRIs and psychotropic medications often used to treat adolescent depression, starting with the FDA approved medications may align best with the comfort level of the general pediatrician.
Additionally, it is important for providers to review the boxed warning (often referred to as the black box warning) with patients and families. The boxed warning stemmed from clinical trials that were conducted in over 4000 children and adolescents where a 2% suicidality risk was identified in those taking the SSRI and in 2% who were given placebo. There were no suicides during these clinical trials.8,15 This information allows providers to educate patients and families that the benefits of initiating medication far outweigh the risks of not treating their child’s depression.
One should aim at achieving the target dose of the SSRI within 3 weeks from initiation. Monitoring medication response should occur every 1 to 2 weeks when starting and visits can be less frequent once the target dose is achieved. Once dosing is optimized, follow up visits for medication management should occur at 2 to 4-month intervals. Families and patients commonly ask how long their teen will need to be on the psychotropic medication. It is best to continue the medication for 6 to 9 months after symptom remission. When the patient is ready for discontinuation, medication should be tapered down 25% per week.4
If the adolescent is not showing positive response with the psychotropic medication it is okay to try the FDA SSRI that you did not try. If you are unable to achieve improvement in mood and functioning after trial of two different medications, one should consider whether they have made the correct diagnosis. This may be the best time to refer the adolescent to a psychiatrist for evaluation and medication management.
When planning for treatment and management of adolescent depression, parents may be hesitant to have their child or teen engage in routine therapy or they may be nervous about having them take a psychotropic medication. Providers should make time to listen and talk with families and patients about the risks and benefits. Combination therapy that includes both therapy and psychotropic medication yields the most benefit however, if the family agrees to start either therapy or medication, this approach can still be beneficial with positive mental health outcomes.4
Providers should aim towards shared decision making. Developing the treatment plan together with the teen and the caregiver to work towards unified goals can optimize mental health outcomes.
REFERENCES
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, (5th ed).
- Anderson M. A Majority of Teens Have Experienced Some Form of Cyberbullying. Pew Research Center. September 27, 2018. Accessed March 1, 2021. https://www.pewresearch.org/internet/2018/09/27/a-majority-of-teens-have-experienced-some-form-of-cyberbullying/
- Centers for Disease Control and Prevention. Adolescent and School Health. Centers for Disease Control and Prevention. Youth Risk Behavior Surveillance System. 2019. Accessed July 10, 2021. https://www.cdc.gov/healthyyouth/data/yrbs/index.htm
- Cheung AH, Zuckerbrot RA, Jensen PS, et al. Guidelines for Adolescent Depression in Primary Care (GLADPC): Part II. Treatment and Ongoing Management. Pediatrics. 2018;141(3).
- Child and Adolescent Mental Health. National Institute of Mental Health. May 2019. Accessed July 10, 2021. https://www.nimh.nih.gov/health/topics/child-and-adolescent-mental-health
- Depression in Children and Adolescents: Screening. U.S. Preventive Services Task Force. Final Recommendation Statement. February 8, 2016. Accessed August 20, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/depression-in-children-and-adolescents-screening
- Downey K, Cross C. Cyberbullying may increase during COVID-19 pandemic, expert says. Healio News. Pediatrics. School Health. March 30, 2020. Accessed August 7, 2021. https://www.healio.com/news/pediatrics/20200330/cyberbullying-may-increase-during-covid19-pandemic-expert-says
- Fornaro M, Anastasia A, Valchera A, et. The FDA “Black Box” Warning on Antidepressant Suicide Risk in Young Adults: More Harm Than Benefits? Frontiers in Psychiatry. 2019; 10:294. doi: 10.3389/fpsyt.2019.0029
- Garland EJ, Kutcher S, Virani A, Elbe D. Update on the Use of SSRIs and SNRIs with Children and Adolescents in Clinical Practice. J Can Acad Child Adolesc Psychiatry. 2016; 25(1): 4-10.
- Heron M. Deaths: Leading Causes for 2016. Natl Vital Stat Rep. 2018 Jul;67(6):1-77. PMID: 30248017.
- How the pandemic has impacted teen mental health. Mott Poll Report. National Poll on Children’s Health. March 15, 2021. Accessed March 30, 2022. https://mottpoll.org/reports/how-pandemic-has-impacted-teen-mental-health
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9, Validity of a Brief Depression Severity Measure. J Gen Intern Med. 2001; 16(9):606-613.
- Parent views on addressing mental health concerns in adolescents. Mott Poll Report. National Poll on Children’s Health. March 21, 2022. Accessed March 30, 2022. https://mottpoll.org/reports/parent-views-addressing-mental-health-concerns-adolescents
- Scott SR, Rivera KM, Rushing E, Manczak EM, Rozek CS, Doom JR. “I Hate This”: A Qualitative Analysis of Adolescents’ Self-Reported Challenges During the COVID-19 Pandemic. Journal of Adolescent Health. 2021; 68(2):262-269.
- Treatment for Adolescents with Depression Study (TADS). National Institute of Mental Health. Accessed March 16, 2022. https://www.nimh.nih.gov/funding/clinical-research/practical/tads#:~:text=The%20NIMH%2Dfunded%20Treatment%20for,adolescents%20ages%2012%20to%2017
- Vannucci A, Simpson E, Gagnon S, Ohannessian CM. Social media use and risky behaviors in adolescents: A meta-analysis. Journal of Adolescence. 2020; 79:258-274.
- Zuckerbrot, RA, Cheung, A, Jensen, PS, Stein, REK, Laraque, D, & GLAD-PC Steering Group. Guidelines for Adolescent Depression in Primary Care (GLAD-PC): Part 1. Practice preparation, identification, assessment, and initial management. Pediatrics. 2018; 141(3), 1–21. https://doi.org/10.1542/peds.2017-4081