A Deceptive Facial Rash
AUTHORS:
Puneet Tung, DO1; Diane Howell, MD2
1Assistant Professor, Department of Pediatrics, Penn State College of Medicine, Hershey, PA
2Assistant Professor, Department of Pediatrics, University of Florida College of Medicine, Gainesville, FL
Case Report | PUBLISHED WINTER 2023 | Volume 43, Issue 1
DOWNLOAD PDF
Introduction
Dermatophyte infections are common in the pediatric population and prevailing causes of fungal infections of hair, skin, and nails. Fungal infections of the epidermis include tinea corporis, tinea pedis, tinea cruris, tinea faciei and tinea manuum. Tinea faciei is an uncommon fungal infection of the face, devoid of terminal hairs, and often presents with clinical symptoms that are usually misdiagnosed. This case illustrates a young girl whose diagnosis and clinical course was prolonged due to misdiagnosis. Prompt recognition of this dermatophyte infection in the pediatric population should be suspected with scaly and pustular eruptions on the face.
Case
A 6-year-old female presented to her pediatrician’s office for the chief complaint of a progressively growing rash on her nose and upper lip that had been present for several weeks. There were also other smaller lesions present on her cheek, chin and forehead (Figure 1). The rash was annular, scaly, dry, and light pink in color. The lesions had well defined borders with a raised pink edge and paler center. There were no others at home who had anything similar. There were several outdoor animal exposures including multiple dogs, a cat and chickens. She is an otherwise healthy 6-year-old, had no significant medical history, and was up to date with all her vaccinations.
She was initially diagnosed with a bacterial infection of the face and treated with a course of topical mupirocin and oral cephalexin. However, when she did not improve after one week, she presented again to her pediatrician’s office and was prescribed a course of mometasone furoate 0.1% and instructed to apply twice daily for one to two weeks for presumptive contact dermatitis. Two weeks later, when the facial lesions still did not improve (Figure 2), she had a fungal culture done and the labs grew Trichophyton species. She was started on butenafine Hcl 1% solution and oral fluconazole. Her facial lesions ultimately resolved approximately six weeks after her initial presentation (Figure 3).
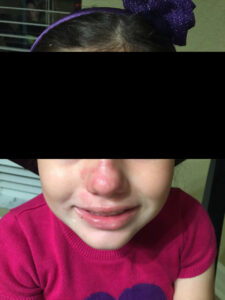 Figure 1: Initial presentation |
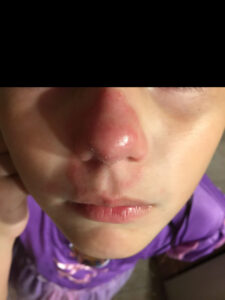 Figure 2: After a course of topical steroids |
 Figure 3: Resolving Dermatophyte Infection |
Diagnosis
Tinea faciei
Discussion
Dermatophytes are the major cause of fungal infections to the skin, hair and nails and are very common.1,2 Dermatophytes are filamentous fungi and belong to the Trichophyton, Microsporum and Epidermophyton genera. Dermatophyte infections classically colonize and metabolize the top layer of skin, the stratum corneum, and reside in the keratin layer of the skin, hair and nails.3,4 The major clinical subtypes of dermatophyte infections include: tinea capitis (head), tinea barbae (beard), tinea corporis (body), and tinea pedis (feet).5 Tinea faciei is a sub-group of tinea corporis that accounts for 3-4% of these infections.6 A typical presentation is an erythematous, annular plaque with scaling, pustules and crusting on the non-bearded region of the face. Additionally, this subtype occurs more frequently in those who live in humid, tropical or subtropical climates.6
The clinician should be suspicious of a cutaneous dermatophyte infection based upon clinical findings. The differential diagnosis of tinea faciei includes granuloma annulare, cutaneous lupus erythematosus, atopic or nummular eczema, seborrheic dermatitis, pityriasis rosea, impetigo, perioral dermatitis and rosacea (Table 1).
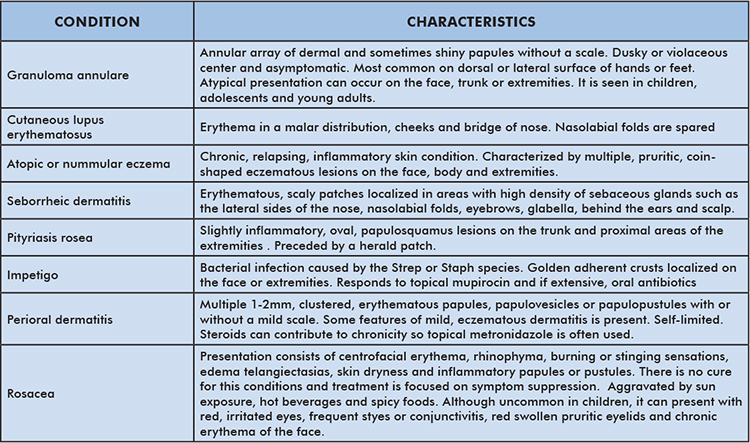
Table 1: Differential Diagnosis of Tinea Faciei
Tinea faciei is observed in both children and adults.6 Individuals who are immunocompromised or who have trisomy 21 have a higher susceptibility to dermatophyte infections. Infection is usually transmitted from contact with infected humans (anthrophilic), animals (zoophilic), soil (geophilic) or fomites (e.g. brushes, combs, towels, hats) as dermatophytes can remain viable for prolonged periods of time.4
While diagnosis is generally made by clinical observation, it can also be confirmed with Potassium hydroxide (KOH) wet mount preparation with direct microscopic examination. This rapid method can be done in most outpatient settings. A fungal culture may also be used to confirm the diagnosis, however it takes 2-4 weeks to process. A sample for either test can be obtained by scraping the moistened, active margin of a lesion with a blunt scalpel, brush or picking at the skin with tweezers. A fungal culture may also be obtained by swabbing the active margin with a cotton-tipped applicator.5,7 Dermatophytes from the genus Microsporum will fluoresce blue-green under Woods lamp and may provide another diagnostic tool.7
Commonly, dermatophyte infections are misdiagnosed, likely due to the infrequent nature and varied presentation of tinea faciei. Nearly 70% of patients are initially misdiagnosed as having an inflammatory skin reaction and treated with topical steroids.8 This modifies the appearance of the dermatophyte infection making the diagnosis more difficult. This phenomenon is known as tinea incognito.4 This altered appearance is characterized by decreased erythema and absence of the typical scaly borders.
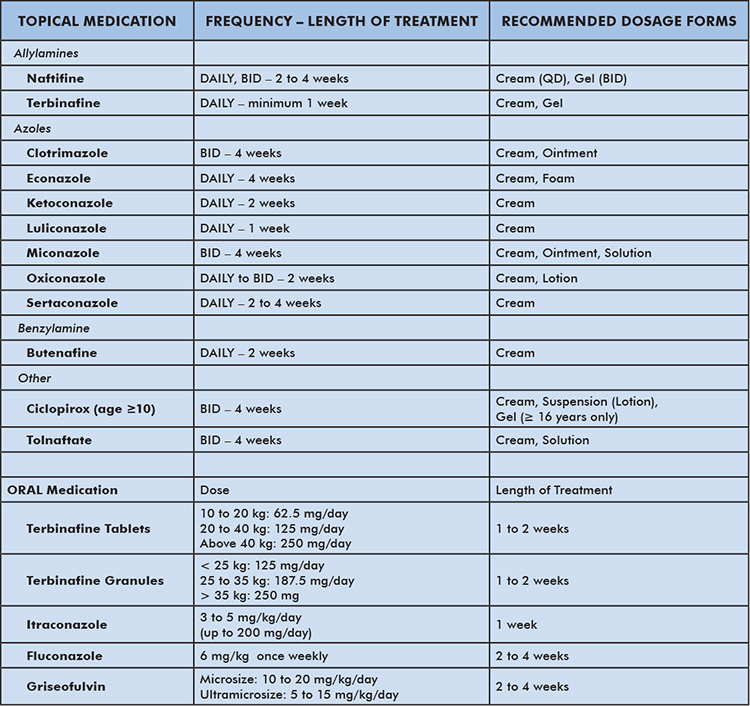
Table 2: Treatments for Tinea Faciei
There is a myriad of effective topical and systemic anti-fungal drugs that can be used as treatments (Table 2). First line therapy can be used for most superficial infections and includes topical therapy with azoles or allylamines such as butenafine, ciclopirox or tolnaftate for two to four weeks. Clinical resolution may be noted by two weeks or earlier, but continuing therapy for two to four weeks is recommended to ensure complete resolution. Oral medications are indicated for extensive and intractable infections that have extended into the dermis, hair follicles or nails. In these cases, Terbinafine, itraconazole, fluconazole and griseofulvin are often prescribed for two to eight weeks.5,7-10
Conclusion
Tinea Faciei is an uncommon superficial dermatophyte infection that is often misdiagnosed and treated as a bacterial infection or an inflammatory skin reaction. Treatment with corticosteroids can further preclude timely diagnosis due to the incognito phenomenon. Fungal infections should always be suspected with scaly eruptions on the face, and both topical and oral treatments are readily available.
References
- Seebacher C, Bouchara JP, Mignon B. Updates on the epidemiology of dermatophyte infections. Mycopathologia. 2008 Nov-Dec;166(5-6):335-52. Epub 2008 May 14. PubMed PMID: 18478365.
- Ameen M. Epidemiology of superficial fungal infections. Clin Dermatol. 2010 Mar 4;28(2):197-201. PubMed PMID: 20347663.
- King A, Balaji S, Keswani SG. Biology and function of fetal and pediatric skin. Facial Plast Surg Clin North Am. 2013 Feb;21(1):1-6. PubMed PMID: 23369584; PMCID: PMC3654382.
- Hawkins DM, Smidt AC. Superficial fungal infections in children. Pediatr Clin North Am. 2014 Apr;61(2):443-55. Epub 2014 Jan 29. PubMed PMID: 24636655.
- Sahoo AK, Mahajan R. Management of tinea corporis, tinea cruris, and tinea pedis: A comprehensive review. Indian Dermatol Online J. 2016 Mar-Apr;7(2):77-86. PubMed PMID: 27057486; PMCID: PMC4804599.
- Lin RL, Szepietowski JC, Schwartz RA. Tinea faciei, an often deceptive facial eruption. Int J Dermatol. 2004 Jun;43(6):437-40. PubMed PMID: 15186226.
- Kimberlin DW, Brady MT, Jackson M. Redbook (2018): Report of the Committee on Infectious Diseases, 31st Edition. AAP Committee on Infectious Diseases. 2018.
- Shapiro L, Cohen HJ. Tinea faciei simulating other dermatoses. JAMA. 1971 Mar 29;215(13):2106-7. PMID: 5108222.
- El-Gohary M, van Zuuren EJ, Fedorowicz Z, Burgess H, Doney L, Stuart B, Moore M, Little P. Topical antifungal treatments for tinea cruris and tinea corporis. Cochrane Database Syst Rev. 2014 Aug 4;(8):CD009992. PubMed PMID: 25090020.
- Dev T, Saginatham H, Sethuraman G. Tinea Faciei: Challenges in the Diagnosis. J Pediatr. 2017 Aug;187:331. Epub 2017 Apr 19. PubMed PMID: 28433202.
