Management of Adolescent Idiopathic Scoliosis: Latest Evidence
AUTHORS:
Yusuf Mehkri, BS1; Eric Panther, BS1; Caroline Davidson1; Jairo Hernandez, BS1; Denna Bakhtiar1; Diane M. Howell, MD2
1University of Florida College of Medicine, Gainesville FL, USA
2Department of Pediatrics, University of Florida College of Medicine, Gainesville FL, USA
Review Article | PUBLISHED SPRING 2023 | Volume 43, Issue 2
DOWNLOAD PDF
Abstract
Adolescent idiopathic scoliosis (AIS) is a structural spinal deformity affecting children >10-years-old without a clear pathogenesis. Appropriate early treatment of AIS is key, as untreated AIS can lead to severe cardiopulmonary dysfunction due to mechanical and structural abnormalities. Patients with mild-to-moderate AIS (10-40°) are treated with non-operative measures while patients with severe AIS (>40°) are treated surgically. Nonsurgical interventions include scoliosis-specific exercises (SSE) and bracing. These measures slowly correct the spinal deformity without the need for surgery. When the spinal deformity is >40°, spinal fusion is presently the standard of care. However, vertebral body tethering and stapling are two fusionless approaches currently undergoing investigation. Pediatric primary care providers should have an awareness of this diagnosis and its evolving treatment options to counsel families and effectively partner with orthopedic specialists in providing optimal patient care.
Introduction
Adolescent idiopathic scoliosis (AIS) is a spinal deformity with both vertebral rotation and a lateral curvature of at least 10° in children of at least ten years of age. AIS is the largest subset of spinal deformities, affecting 1-4% of adolescents between the age of 10 and skeletal maturity.1 The need for intervention depends largely on the magnitude and progression of the curve, since the presumption is that greater curve magnitude is associated with increased risk of future negative physical and psychological consequences. These include decreased pulmonary function, increased back pain, psychosocial difficulties and decreased quality of life.2 The level of intervention in the current management of AIS depends on both the severity of the curvature as measured by the Cobb angle and future growth potential of the patient’s spine. Pediatric primary care providers must partner with orthopedic specialists to care for these patients, and an awareness of current diagnostic and therapeutic approaches is useful to primary care providers as they assess and counsel patients.
Scoliosis specific exercise (SSE) are typically recommended for patients with primary curve angles measuring 10-40° a with the goals of developing awareness of self-correcting postures and encouraging muscle strength to enhance the effects of a brace. Bracing is also recommended to these patients with the goal that the external corrective forces of the brace will halt curve progression and eliminate the need for surgical treatment in the future.3 For patients with severe AIS, defined by curve magnitude ≥40° and skeletal immaturity, surgery is the standard of care. The gold standard for surgery is spinal fusion with pedicle screw fixation, as severe AIS can progress to cardiopulmonary dysfunction due to mechanical dysfunction of the thoracic cavity.4,5 The two main goals of surgery are: 1) maximize curve correction and minimize curve progression to avoid the aforementioned health risks, and 2) ensure that functional mobility and flexibility are optimized. Over the past decade alone, surgical advancements, improved radiographic techniques, and superior functional outcomes for patients have emerged. This review article will provide an overview of the latest evidence on non-surgical and surgical management of AIS.
Nonsurgical Interventions
Patients with curve angles of less than 10° do not meet the criteria for an AIS diagnosis. Patients with curve angles of 10-25°
are considered to have mild AIS and will generally be monitored with serial x-rays at 3-, 6-, or 12-month intervals. Those with moderate AIS have curve angles of 25-40° and will also undergo serial x-rays to track the progression of their scoliosis. Besides watchful
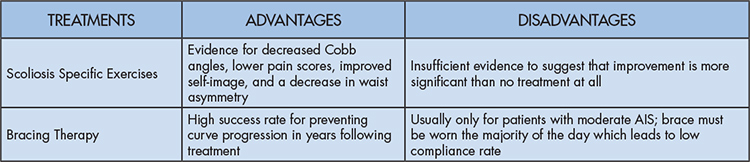
waiting, nonsurgical interventions for patients with mild to moderate AIS (10-40°) include scoliosis-specific exercises (SSE) and bracing (Table 1).
In mild to moderate AIS, specific exercises are both as an adjunct and alternative to bracing. There are many SSE regimens around the world, with some notable ones including the Scientific Approach to Scoliosis from Italy and the Schroth approach from Germany, which are scoliosis-specific intensive inpatient rehabilitation programs with certified therapists.6 The exercise prescription and regimen depend on the severity of curve. However, all regimens include both static and dynamic movements. Exercises recommended for all curve types include a “side-lying shoulder contraction” where the patient lies on their side with their waist elevated by a high-density foam roller. Other exercises require the patient to practice balancing on a stability ball or practice “conscious walking”, walking while auto-correcting spinal asymmetry.7 These SSE regimens have been assessed in randomized controlled trials with impressive results, including decrease in Cobb angles, lower pain scores, improved self-image, and a decrease in waist asymmetry.8 However, reviews have shown that there is insufficient evidence to suggest that the Schroth and the Scientific Approach to Scoliosis improve outcomes in AIS compared to no intervention.9 There is a need for more and varied studies investigating the effectiveness of SSEs in improving spinal curvature in AIS patients.
Bracing therapy is primarily indicated for patients with moderate AIS (curve angle: 25-40°) to prevent the scoliosis from progressing over time. Most bracing recommendations suggest the brace should be worn at least 16 hours per day, with the treatment protocol lasting from 2 to 4 years or until skeletal maturity. Although these braces are widely prescribed, these devices have low compliance rates.10 At present, the literature remains inconclusive with respect to the efficacy of bracing for skeletally immature adolescents with mild AIS. Danielson et al.11 conducted a 16-year follow-up study of 92 moderate AIS patients and found no curve progression in patients primarily treated with a brace, but an average curve progression of 6° for the 70% of patients in the observational group who were not treated surgically or with a brace. On the other hand, a meta-analysis by Dolan and Weinstein12 found no significant difference between surgical rates after bracing compared to observation. Given the intense time requirement and discomfort of brace treatment, it is not surprising that noncompliance is one of the most prevalent risk factors in the progression of scoliosis. Although the results for bracing therapy effectiveness are mixed, a recent meta-analysis showed that adding SSE to bracing therapy improved patient outcomes compared to bracing alone.13 Rigorous, prospective studies of the individual and combined effectiveness of bracing and SSEs on curve progression and occurrence of surgical intervention are needed.
Surgical Intervention
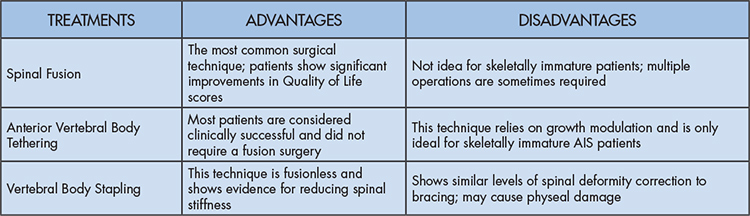
Spinal fusion
Currently, the most common surgical approach for the treatment of AIS is posterior spinal fusion (PSF). PSF allows for a strong, stable correction of severe AIS, while providing significant improvements in all domains of the Health-Related Quality of Life (SRS-30) questionnaire among adolescents with all types of AIS.14 A caveat is that this procedure is not the best option for a subset of patients who are skeletally immature and experience progressive angular and rotational spinal deformity (also known as the crankshaft phenomenon) after undergoing PSF. This phenomenon occurs because the anterior elements of the spine continue to grow in patients with high growth potential who undergo posterior-only fusion.15 Potential adverse outcomes include impairment of pulmonary function and revision surgery, which can be avoided with a combined anterior and posterior fusion approach (APSF).15 Sponseller et al.16 conducted a two-year follow-up on 29 skeletally immature patients who had undergone either PSF or APSF. They showed that although the APSF group had significantly longer hospital stay and operative time, this group had no patients go on to >10° curve progression as compared to 35% of patients in the PSF group. For the general AIS patient population, when it comes to deciding between performing either PSF or APSF, a recent meta-analysis looked at 872 patients across ten studies from 1976 to 2013 and found the two to be equally effective when it came to curve correction. However, the posterior-only approach also showed significantly less blood loss, fewer complications, shorter operative and recovery time, and a level of effectiveness that deemed an additional anterior surgical intervention unnecessary.17
Minimally invasive spinal surgery (MIS), which employs smaller incisions in order to minimize injury to the paraspinous muscles and other structures, has also shown promising results and may become an alternative to the gold standard in the coming years. This approach has long been effective for adult spine pathologies and deformities and has just started to make its way to the AIS population.18 Sarwahi et al.19 showed that patients who underwent MIS achieved comparable curve correction and accurate screw placement as patients who underwent PSF. However, there was no difference in level of pain or hospital stay as was expected. Zhu et al.20 carried out a similar study soon after with AIS patients and obtained better results including decreased radiation exposure, blood loss, and post-operative pain. Although both studies did show a significantly longer operation time for MIS, this can be partially attributed to the inherent learning curve. As more surgeons are trained in MIS, and more long-term data is collected, this technique may become more effective at treating the technically challenging spinal deformities of AIS patients.
Anterior Vertebral Body Tethering
Anterior vertebral body tethering (VBT) is a fusionless approach to treating AIS patients by slowing down vertebral growth on the convex side in the hopes of equilibrating the height on both sides of the vertebral body.21 Newton et al.22 showed that asymmetric spinal tethering can result in growth modulation and spinal deformity in an immature bovine model, and another study23 showed that pre-tensioning of the tether can modulate growth while maintaining disc health, spinal motion, and stiffness. Because this technique relies on growth modulation, it is ideal for skeletally immature AIS patients with flexible curves.
Samdani et al.24 was the first group to retrospectively evaluate outcomes with a large cohort (n=32) of AIS patients and found very promising results. At one-year follow-up, there was a 58% decrease in thoracic curve magnitude and an average 6° reduction in thoracic axial rotation. A two-year follow-up was conducted on eleven of these patients showing further progressive improvements in both measures.25 Overcorrection was a concern in a few patients who had to undergo revision surgery to loosen the tether, however, this was expected given the early experimental nature of this procedure. Takahashi et al.26 performed a study with 23 adolescent idiopathic scoliosis patients which determined the rate of kyphosis correction to be approximately 1.8° per segment per year for the first 2-3 years following anterior VBT.
Newton et al.27 conducted a two to four-year follow-up and obtained interesting results. Although 59% of the 17 patients studied were considered clinically successful because they had achieved curves measuring <35° and did not require PSF, many patients either underwent revision surgery for tether-related issues or experienced curve progression around 18 months post-operation. The authors used these findings to suggest that more data ≥ 2 years post-operation and up to skeletal maturity are necessary to better understand how patients respond to VBT. It is important to keep in mind that three patients included in this study had syndromic scoliosis (not idiopathic), and that most of these patients would not have been considered ideal candidates for VBT considering their curves demonstrated <50% flexibility.21 Newton et al.27 more recently demonstrated in a 14-patient study of all idiopathic scoliosis patients that anterior VBT can cause the periapical vertebrae and discs to grow asymmetrically leading to the desired reduction in disc height on the convex side.
Vertebral Body Stapling
Vertebral Body Stapling (VBS) is another proposed fusionless technique for correction of AIS.28 This procedure is performed by placing staples on the anterior vertebral growth plates causing restrained growth on the convex side and natural growth on the concave side of the spine.4 Sunni et al.28 evaluated the efficacy of VBS in bovine calves and showed that VBS appears to reduce spinal stiffness but can cause physeal damage. However, Murray et al.29 evaluated 7 patients with AIS who underwent VBS for correction of their spinal curvature. The average rate of growth on the stapled verses unstapled side were 0.86 mm/year and 0.83 mm/year respectively. This similar rate of growth demonstrates that in its current form VBS cannot be used for severe scoliosis. Trupia et al.30 concluded in a 10 AIS patient study that VBS does not appear to be more beneficial than bracing. VBS also did not affect the percentage of patients who eventually required surgical intervention for their worsening scoliosis. Additionally, they showed that VBS and bracing resulted in similar levels of spinal deformity correction. In conclusion, VBS does not currently appear to be not a viable option for surgically correcting AIS because it delays adequate treatment (Table 2).
Conclusion
Adolescent idiopathic scoliosis impacts many children between the age of 10 to skeletal maturity and is associated with pulmonary dysfunction, back pain, and negative psychosocial consequences. Treatment over the last decade has largely been posterior spinal fusion which requires instrumentation and considerable risk of revision surgery, increasing the risk of infection and complications. However, novel nonsurgical and surgical treatments have recently emerged as promising therapeutics for AIS. Scoliosis specific exercises appear to help with deformity and pain in patients with moderate scoliosis, whereas bracing therapy has demonstrated mixed results. The combination of the two has been shown to be effective. Surgical treatment appears to be moving away from traditional posterior spinal fusion and toward minimally invasive approaches to the procedure as well as novel vertebral body tethering due to its high success rate and lower risk of complications. The treatment method physicians propose to their patients should be tailored to the patient’s unique clinical picture and goals. Pediatric primary care providers should be aware of current research outcomes and treatment trends to assist in referring patients for the most evidence-based care.
References
- Cheng JC, Castelein RM, Chu WC, et al. Adolescent idiopathic scoliosis. Nat Rev Dis Primers. 2015;1:15030. doi:10.1038/nrdp.2015.30
- Weinstein SL. The Natural History of Adolescent Idiopathic Scoliosis. J Pediatr Orthop. 2019;39(Issue 6, Supplement 1 Suppl 1):S44-S46. doi:10.1097/BPO.0000000000001350
- Richards BS, Bernstein RM, D’Amato CR, Thompson GH. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine (Phila Pa 1976). 2005;30(18):2068-2075; discussion 2076-2077. doi:10.1097/01.brs.0000178819.90239.d0
- Cheung ZB, Selverian S, Cho BH, Ball CJ, Kang-Wook Cho S. Idiopathic scoliosis in children and adolescents: emerging techniques in surgical treatment. World Neurosurg. 2019;130:e737-e742. doi:10.1016/j.wneu.2019.06.207
- Tambe AD, Panikkar SJ, Millner PA, Tsirikos AI. Current concepts in the surgical management of adolescent idiopathic scoliosis. Bone Joint J. 2018;100-B(4):415-424. doi:10.1302/0301-620X.100B4.BJJ-2017-0846.R2
- Berdishevsky H, Lebel VA, Bettany-Saltikov J, et al. Physiotherapy scoliosis-specific exercises – a comprehensive review of seven major schools. Scoliosis Spinal Disord. 2016;11:20. doi:10.1186/s13013-016-0076-9
- Schreiber S, Parent EC, Moez EK, et al. The effect of Schroth exercises added to the standard of care on the quality of life and muscle endurance in adolescents with idiopathic scoliosis-an assessor and statistician blinded randomized controlled trial: “SOSORT 2015 Award Winner.” Scoliosis. 2015;10:24. doi:10.1186/s13013-015-0048-5
- Kuru T, Yeldan İ, Dereli EE, Özdinçler AR, Dikici F, Çolak İ. The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: a randomised controlled clinical trial. Clin Rehabil. 2016;30(2):181-190. doi:10.1177/0269215515575745
- Day JM, Fletcher J, Coghlan M, Ravine T. Review of scoliosis-specific exercise methods used to correct adolescent idiopathic scoliosis. Arch Physiother. 2019;9:8. doi:10.1186/s40945-019-0060-9
- Kim W, Porrino JA, Hood KA, Chadaz TS, Klauser AS, Taljanovic MS. Clinical evaluation, imaging, and management of adolescent idiopathic and adult degenerative scoliosis. Curr Probl Diagn Radiol. 2019;48(4):402-414. doi:10.1067/j.cpradiol.2018.08.006
- Danielsson AJ, Hasserius R, Ohlin A, Nachemson AL. A prospective study of brace treatment versus observation alone in adolescent idiopathic scoliosis: a follow-up mean of 16 years after maturity. Spine (Phila Pa 1976). 2007;32(20):2198-2207. doi:10.1097/BRS.0b013e31814b851f
- Dolan LA, Weinstein SL. Surgical rates after observation and bracing for adolescent idiopathic scoliosis: an evidence-based review. Spine (Phila Pa 1976). 2007;32(19 Suppl):S91-S100. doi:10.1097/BRS.0b013e318134ead9
- Li K, Miao J, Zhang J. Network meta-analysis of short-term effects of different strategies in the conservative treatment of AIS. Eur J Med Res. 2021;26(1):54. doi:10.1186/s40001-021-00526-6
- Rodrigues LMR, Gotfryd AO, Machado AN, Defino M, Asano LYJ. Adolescent idiopathic scoliosis: surgical treatment and quality of life. Acta Ortop Bras. 2017;25(3):85-89. doi:10.1590/1413-785220172503157788
- Murphy RF, Mooney JF. The Crankshaft phenomenon. J Am Acad Orthop Surg. 2017;25(9):e185-e193. doi:10.5435/JAAOS-D-16-00584
- Sponseller PD, Jain A, Newton PO, et al. Posterior spinal fusion with pedicle screws in patients with idiopathic scoliosis and open triradiate cartilage: does deformity progression occur? J Pediatr Orthop. 2016;36(7):695-700. doi:10.1097/BPO.0000000000000524
- Chen Z, Rong L. Comparison of combined anterior-posterior approach versus posterior-only approach in treating adolescent idiopathic scoliosis: a meta-analysis. Eur Spine J. 2016;25(2):363-371. doi:10.1007/s00586-015-3968-0
- Urbanski W, Zaluski R, Kokaveshi A, Aldobasic S, Miekisiak G, Morasiewicz P. Minimal invasive posterior correction of Lenke 5C idiopathic scoliosis: comparative analysis of minimal invasive vs. open surgery. Arch Orthop Trauma Surg. 2019;139(9):1203-1208. doi:10.1007/s00402-019-03166-y
- Sarwahi V, Galina JM, Hasan S, et al. Minimally invasive versus standard surgery in idiopathic scoliosis patients: a comparative study. Spine (Phila Pa 1976). 2021;46(19):1326-1335. doi:10.1097/BRS.0000000000004011
- Weiguo Zhu, Weixiang Sun, Leilei Xu, et al. Minimally invasive scoliosis surgery assisted by O-arm navigation for Lenke Type 5C adolescent idiopathic scoliosis: a comparison with standard open approach spinal instrumentation. J Neurosurg Pediatr. 2017;19(4):472-478. doi:10.3171/2016.11.PEDS16412
- Boudissa M, Eid A, Bourgeois E, Griffet J, Courvoisier A. Early outcomes of spinal growth tethering for idiopathic scoliosis with a novel device: a prospective study with 2 years of follow-up. Childs Nerv Syst. 2017;33(5):813-818. doi:10.1007/s00381-017-3367-4
- Newton PO, Fricka KB, Lee SS, Farnsworth CL, Cox TG, Mahar AT. Asymmetrical flexible tethering of spine growth in an immature bovine model. Spine (Phila Pa 1976). 2002;27(7):689-693. doi:10.1097/00007632-200204010-00004
- Newton PO, Farnsworth CL, Upasani VV, Chambers RC, Varley E, Tsutsui S. Effects of intraoperative tensioning of an anterolateral spinal tether on spinal growth modulation in a porcine model. Spine (Phila Pa 1976). 2011;36(2):109-117. doi:10.1097/BRS.0b013e3181cc8fce
- Samdani AF, Ames RJ, Kimball JS, et al. Anterior vertebral body tethering for immature adolescent idiopathic scoliosis: one-year results on the first 32 patients. Eur Spine J. 2015;24(7):1533-1539. doi:10.1007/s00586-014-3706-z
- Samdani AF, Ames RJ, Kimball JS, et al. Anterior vertebral body tethering for idiopathic scoliosis: two-year results. Spine (Phila Pa 1976). 2014;39(20):1688-1693. doi:10.1097/BRS.0000000000000472
- Takahashi Y, Saito W, Yaszay B, Bartley CE, Bastrom TP, Newton PO. Rate of scoliosis correction after anterior spinal growth tethering for idiopathic scoliosis. J Bone Joint Surg Am. 2021;103(18):1718-1723. doi:10.2106/JBJS.20.02071
- Newton PO, Kluck DG, Saito W, Yaszay B, Bartley CE, Bastrom TP. Anterior Spinal growth tethering for skeletally immature patients with scoliosis: a retrospective look two to four years postoperatively. J Bone Joint Surg Am. 2018;100(19):1691-1697. doi:10.2106/JBJS.18.00287
- Sunni N, Askin GN, Labrom RD, Izatt MT, Pearcy MJ, Adam CJ. The effect of vertebral body stapling on spine biomechanics and structure using a bovine model. Clin Biomech (Bristol, Avon). 2020;74:73-78. doi:10.1016/j.clinbiomech.2020.02.006
- Murray E, Tung R, Sherman A, Schwend RM. Continued vertebral body growth in patients with juvenile idiopathic scoliosis following vertebral body stapling. Spine Deform. 2020;8(2):221-226. doi:10.1007/s43390-019-00019-x
- Trupia E, Hsu AC, Mueller JD, Matsumoto H, Bodenstein L, Vitale M. Treatment of idiopathic scoliosis with vertebral body stapling. Spine Deform. 2019;7(5):720-728. doi:10.1016/j.jspd.2019.01.006